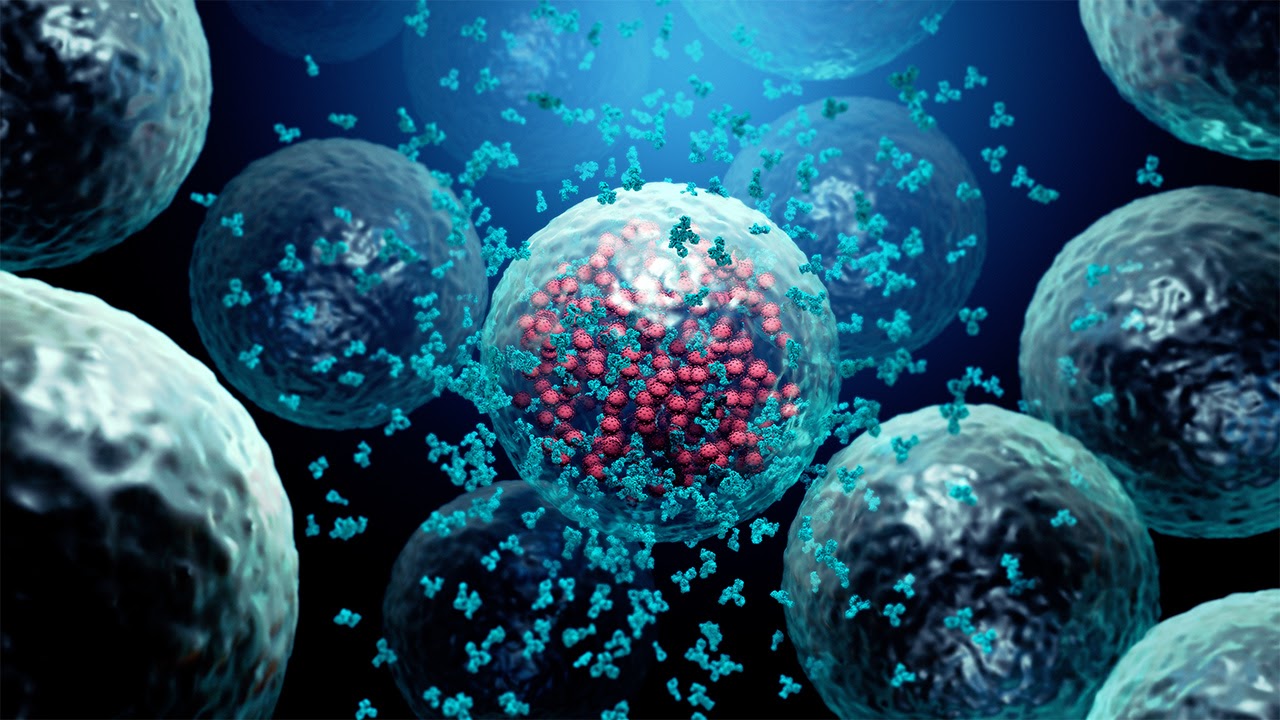
The severe acute respiratory syndrome, also known as SARS-CoV-2 or the Covid-19 has caused unusual global health and economic dilemmas. Numerous vaccine strategies and repurposed drugs are currently under evaluation for safety and efficiency. Meanwhile, diverse neutralizing monoclonal antibodies (nMAbs) targeting SARS-CoV-2 spike glycoprotein are in diverging stages of clinical trials and antibody development.
Preclinical researches have revealed that a mix of potent nMAbs targeting the receptor-binding site of SARS-CoV-2 and broad nMAbs targeting conserved regions in the virus spike might be practical for the medication and prevention of SARS-CoV-2 infection.
In contradiction to SARS-CoV, which was initially reported in 2003 and characterised by restrictive human-to-human transmission, SARS-CoV-2 has expanded exponentially and has led to more than 1.3 million mortalities from COVID-19, 11 months following its identification. SARS-CoV-2 and SARS-CoV, which pertain to the beta-CoV genera of Coronaviridae, share the same receptor — angiotensin-converting enzyme 2 for viral entry into host cells through the spike proteins on the virus’ surface. For both viruses, the SARS-CoV-2 spike protein consists of S1 and S2 subunits.
The receptor-binding domain (RBD) in the S1 sub-unit primarily joins the ACE2 receptor on the cells to intercede viral entry via the RBD–ACE2 complex formation. The S proteid then encounters a conformational change, leading to a membrane coalition arbitrated by the S2 sub-unit. The S protein produces a homotrimer and can experience spontaneous alternatives with individual or more RBDs, changing from a ‘lying down’ position to a ‘standing up’ position to enable receptor binding.
The structural proteins of SARS-CoV-2 — i.e., S, nucleocapsid (N), membrane (M), and envelope (E) — perform crucial functions in viral infection and replication2. Therefore, knowing the structure and function of these proteins, particularly of the S protein and its RBD, presents a basis for the systematic design and development of SARS-CoV-2-specific nAbs for protective prevention and treatment of COVID-19.
Neutralizing antibodies (nAbs) can be indifferently transferred into individuals before or following viral infection to treat or prevent disease. Therapeutic nAbs generally subsist in the body for a short time and their potential treatment efficacy relies on a mixture of factors, including nAb titer, total amount, particularity and half-life. Neutralizing antibody therapies with significant specificity, active affinity to target proteins, and low toxicity have been used to treat viral infections caused by the Ebola virus, cytomegalovirus, influenza virus, human immunodeficiency virus, and respiratory syncytial virus.
There are striking differences between neutralizing Monoclonal antibodies and nanobodies. Monoclonal antibodies and their remnants usually are significant to sustain their conformation and functionality. Most have to be manufactured in mammalian cell expression systems, which typically have a comparatively low expression yield and high production costs. In opposition, nanobodies are single-domain antibodies with small size, good solubility and strong stability against extreme conditions.
They can be quickly produced in Escherichia coli and yeast cells at a large scale, resulting in a high expression yield, great functionality, and considerably diminished production costs. Small size nanobodies typically have higher renal clearance and a shorter half-life than mAbs. Yet, nanobodies can usually increase half-life by fusing them with long-lived proteins, such as albumin or human fragment crystallisable (Fc) region. Overall, it is vital to consider the production cost, stability and half-life of nAbs in addition to their efficacy and safety.
Antibody generation response in COVID-19 patients
In COVID-19 patients, viral load peak occurs concomitantly or shortly after symptoms onset. After peaking, viral load decreases slowly and is detectable for up to 4 weeks. However, the infective virus has been isolated from the upper respiratory tract only within the first week after symptom onset.
As the virus replicates, the adaptive immunity is stimulated to generate cellular responses and antibody generation, including NAbs in most SARS2 infected symptomatic individuals. IgM, IgG and IgA antibodies directed to SARS2 external S and internal N proteins develop within the first week after the onset of symptoms and peak two weeks after the symptoms show up.
In 50 per cent of individuals, seroconversion occurs one week after symptoms onset and 100% of individuals seroconvert by the end of the second week after symptom development. Several studies reported an inverse correlation between viral loads and SARS2 specific-antibodies; however, by the time that Abs develop, viral loads have already started to decrease, indicating that innate and cellular adaptive immunity contributes to the initial virus containment.
Additionally, the antibody response can be weak or absent in asymptomatic or mild infections, suggesting partial control of the virus by innate or T-cell mediated immunity. Paradoxically, several studies have found a positive correlation between specific antibody titers and disease severity, suggesting that a robust Ab response alone is insufficient to avoid severe disease. Studies have also pointed out that the timing of antibody development might be crucial to neutralize the virus control.
Development of monoclonal antibodies (nMAbs) for COVID-19
Several monoclonal antibodies (MAbs) targeting the RBS of SARS1 have been described (i.e., CR3014, M396 and S230). Although these MAbs effectively neutralize SARS Cov-2 variants, most of them do not cross balance SARS2 due to discrepancies in the primary amino acid sequence of RBS among these viruses. However, these observations supported the discovery and characterisation of SARS2 MAbs from COVID-19 patients.
Over the last two decades, several programs from several institutions have established the platforms and enabled HIV vaccine development and agile responses to viral pandemics. Those and other global initiatives have teams and technologies that are now responding to the COVID-19 pandemic to confine SARS2 needs.
Avoiding the emergence of virus resistance.
A natural mutation of SARS2 has now been detected at residue, which forms part of the ACE2 binding epitope. As RNA viruses are known to accumulate mutations over time, a big concern for any antiviral treatment is the high-risk of selecting potential treatment-induced escape emergent variants.
In this regard, the discovery of novel nMAbs targeting different sites on SARS2 S protein will be significant to counteract the mutational capacity of the virus and avoid the emergence of resistant viral variants due to the administration of single-drug therapy. One approach to prevent viral escape would be using antibodies targeting highly conserved epitopes on S protein.
Contact Helvetica Health Care to Buy Monoclonal and Polyclonal Antibodies