Antibodies are proteids the body produces when a disease occurs; they connect to a virus and support eliminating it. A monoclonal antibody is an antibody generated by cloning a selective white blood cell. Antibodies can be monoclonal or polyclonal. It is procured from a one-cell clone which is a single B cell clone.
All subsequently derived antibodies are outlined back to their distinctive parent cell in this way. Consequently, a single, unadulterated form of antibody is a monoclonal antibody. Monoclonal antibodies are concentrated forms of distinct antibodies that function against coronavirus.
How do monoclonal and Polyclonal antibodies work against COVID-19?
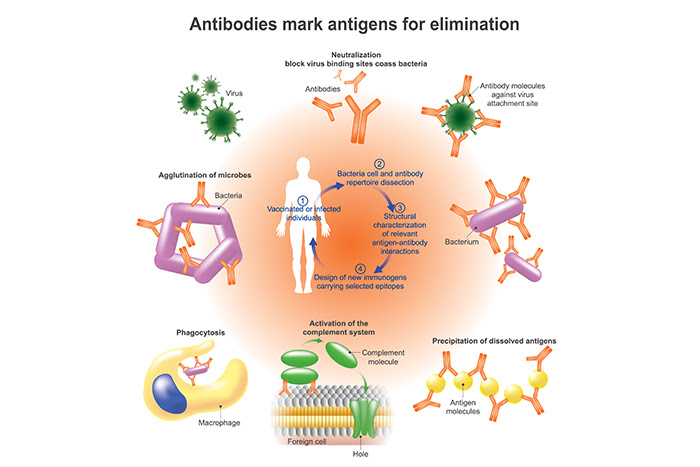
Monoclonal antibodies against COVID-19 append to the virus to block it from penetrating human cells. The monoclonal antibody protein also traces whether the immune system’s virus is broken down and cleared from the body. Researchers leverage the natural human immune response to generate next-generation, whole human polyclonal antibody therapeutics without the need for human serum, extending both the safety and potency. These highly productive antibodies have proven to neutralise and block disease and also address future mutations.
Polyclonal antibodies (pabs) are heterogeneous compounds produced naturally by different B cell clones in the body. In monoclonal antibodies, there is monovalent affinity, restricted only to the same or single epitope the antibody is a known element of the antigen. By contradiction, polyclonal antibodies bind to multiple epitopes.
The effectiveness and safety of this investigational therapy continue to be evaluated for the treatment of COVID-19. The investigational monoclonal antibody therapy treats mild-to-moderate COVID-19 in grown-ups and pediatric patients with positive outcomes of direct SARS-CoV-2 viral trial and who are at high risk for progression to critical COVID-19, including hospitalisation or mortality.
Therapies authorised for COVID-19.
To date, four monoclonal antibodies targeting the SARS-CoV-2 spike protein have been authorised for use to treat high-risk outpatients who have a mild-to-moderate disease to limit progression to intractable illness. These four monoclonal antibodies approved are called bamlanivimab, etesevimab, casirivimab, and imdevimab.
There is an ever-widening focus on replacing CPT with counterbalancing mAbs, where dosing to assure the appropriate neutralising capacity of the antibodies can be more definite. Presently, the mass-produced recombinant mAbs has become extensible to meet demand and is cost-competitive with other treatments. Neutralising mAbs subdues limitations fundamental to CPT.
Furthermore, a high titre of counterbalancing antibodies — which current evidence indicates is essential for the effectiveness of CPT — is integrated into neutralising mAbs. As of March 2021, at least 20 neutralising mAb therapies were being tested in current stage clinical trials or had previously been approved for application in nine transmissible diseases, including RSV infection and Ebola.
Monoclonal and polyclonal antibodies have many advantages as they reduce viral levels and the resulting damage to the lungs. Monoclonal antibodies enhanced symptoms in non-hospitalised covid-19 patients and allowed non-hospitalised patients to heal more rapidly. This treatment is only carried out in people who did not have immunoglobulins to SARS-CoV-2; it has also worked better on individuals/cases with higher virus levels.
There are about two or more lab directed antibodies used in the polyclonal antibody cocktail treatment. The monoclonal antibody attacks the spike protein used by the virus to dig into good cells and another antibody that invades another element of the coronavirus. The drug’s objective is to stop the reproduction of the virus or its variants. The purpose of multiple antibodies being consolidated is to prevent mutations seen with individual antibodies from escaping.
Modern global collaboration to control SARS-CoV-2 outbreak
The sequence of the SARS-CoV-2 genome has also facilitated the evolution of polymerase chain reaction (PCR) based diagnostics that can be induced to the front lines and leveraged to distinguish infected individuals instantly. These experiments are vital to both patient management and rate tracking, so execution must be profoundly accurate.
The FDA declared emergency application and authorisation, enabling the deployment of the CDC reagents to laboratories across the U.S. The Centers for Disease Control (CDC) and the Food and Drug Administration (FDA) in the U.S. worked similarly promptly on a PCR diagnostic panel for SARS-CoV-2. In Europe, the European Center for Disease Control (ECDC) also suggests PCR-testing for the SARS-CoV-2.
Researchers are expecting that monoclonal antibodies might help to prevent and treat new symptoms of Covid-19 infections. Since they emanate in the blood of people who have recovered from Covid-19, they can directly target the SARS-CoV-2 virus. When authorised, they will render fast protection against infection, as monoclonal antibodies enter the bloodstream immediately.
Researchers anticipate that monoclonal antibodies will balance and complement covid-19 vaccines to constrain the pandemic. Monoclonal antibodies can treat all people, including the aged, adolescents, children, and even immunocompromised individuals.
Visit Helvetica Health Care to discover a comprehensive range of monoclonal and polyclonal antibodies against infectious agents.